Melasma

What is Melasma?
For most, melasma is frustrating. It appears as patches of discoloration on the skin, varying from light to dark. Melasma is most common in women, typically showing up on the face, although it can occasionally appear on other parts of the body.
Even though some women may be genetically predisposed to melasma, both internal and external factors can trigger or worsen it.
Internal Factors and Melasma
Hormones are a major internal factor linked to melasma. Pregnancy and birth control pills are the most common hormonal triggers. This is why melasma is sometimes referred to as the "mask of pregnancy." During pregnancy, the surge in estrogen and progesterone levels can overstimulate melanocytes (the skin cells responsible for pigment production), leading to uneven skin tone.
Other hormonal imbalances, such as thyroid issues or hormonal replacement therapy (HRT), can also contribute to melasma. Stress is another overlooked internal factor, as increased cortisol levels (the stress hormone) can disrupt hormonal balance and trigger pigmentation issues.
External Factors and Melasma
While external factors don’t directly cause melasma, they can worsen it by stimulating melanocytes. The biggest external culprits are:
- UV Radiation: Sun exposure is the most significant trigger for melasma. UV rays penetrate the skin and stimulate melanocytes, leading to increased pigment production and darkening of existing patches.
- Heat: High temperatures can also activate melanocytes, even if you’re not directly in the sun. This includes heat from the sun, hot showers, saunas, and even cooking over a stove.
- Skincare Products and Treatments: Harsh exfoliants, certain acids, and irritating skincare products can cause inflammation, which may lead to increased melanin production.
- Blue Light: Light from phone, computer, and tablet screens can also contribute to pigmentation. It’s important to protect your skin with antioxidant-rich products and blue light-blocking ingredients.
Excess Oil and Inflammation
Excess sebum (oil) in the skin can increase inflammation, which in turn stimulates melanocytes. People with oily or acne-prone skin are at a higher risk of developing melasma because inflammation from breakouts or clogged pores can trigger pigmentation.
Controlling oil production with the right skincare products, such as salicylic acid or niacinamide-based formulas, can help reduce inflammation and prevent melasma from worsening.
How to Manage and Treat Melasma
Even though melasma has no permanent cure, it can be controlled and managed with a targeted skincare routine and professional treatments. The key is to combine products and treatments that control inflammation, regulate melanin production, and protect the skin from external triggers.
1. Sun Protection is Non-Negotiable
Daily sunscreen use is essential for managing melasma. A broad-spectrum sunscreen with SPF 30 or higher should be applied every morning and reapplied every two hours when outdoors. Physical sunscreens (with zinc oxide or titanium dioxide) are often more effective for melasma-prone skin because they reflect UV rays rather than absorbing them.
Look for sunscreens that also provide protection from blue light and infrared heat, which can worsen melasma. Tinted sunscreens with iron oxides are especially beneficial, as they protect against visible light that can stimulate pigmentation.
2. Tyrosinase Inhibitors to Prevent Pigment Production
Tyrosinase is the enzyme that controls melanin production. Tyrosinase inhibitors work by blocking this enzyme, helping to prevent new pigmentation from forming. Effective tyrosinase inhibitors include:
- Hydroquinone (prescription-strength)
- Kojic Acid
- Tranexamic Acid
- Vitamin C
- Arbutin
- Licorice Extract
If you’re considering chemical peels or laser treatments for melasma, it’s important to be on a tyrosinase inhibitor beforehand. This prevents melanocytes from being overstimulated and reduces the risk of rebound pigmentation.
3. Prescription Protocols for Stubborn Melasma
The most effective treatment for melasma is a 3–5 month prescription protocol that includes 4% hydroquinone (to lighten pigmentation) and tretinoin (to increase skin cell turnover). After completing the protocol, take a break for at least two months and switch to non-hydroquinone products to maintain results and prevent long-term damage.
Long-term use of hydroquinone without breaks can lead to Ochronosis, a condition where the skin becomes thick and blue-black in color. That’s why pulse therapy — alternating hydroquinone with non-hydroquinone treatments — is recommended to prevent side effects.
4. Exfoliation and Skin Renewal
Gentle exfoliation helps improve melasma by removing surface pigmentation and encouraging new skin cell growth. Use mild exfoliants like lactic acid or mandelic acid 1–2 times per week. Avoid harsh scrubs or over-exfoliating, as this can increase inflammation and worsen pigmentation.
5. Hydration and Skin Barrier Repair
A compromised skin barrier makes melasma harder to treat because it allows more environmental stressors (like UV and pollution) to penetrate the skin. Strengthen your skin barrier with:
- Ceramides
- Hyaluronic Acid
- Fatty Acids
- Peptides
Keeping the skin hydrated and nourished helps reduce inflammation and supports overall skin health, making melasma easier to manage.
What to Avoid with Melasma
- Hot Water: Hot showers and steam rooms can increase blood flow to the skin, stimulating melanocytes.
- Fragranced or Irritating Products: Fragrance and harsh chemicals can cause inflammation and worsen melasma.
- Excessive Exfoliation: Over-exfoliating can trigger inflammation, leading to more pigmentation issues.
- Hormonal Imbalance: Work with your doctor to address any underlying hormonal issues that may be contributing to melasma.
Professional Treatments for Melasma
For more stubborn cases of melasma, professional treatments can enhance results:
- Chemical Peels – A series of mild chemical peels with glycolic acid, lactic acid, or mandelic acid can help lighten pigmentation and improve skin texture.
- Microneedling with Tranexamic Acid – This treatment helps deliver skin-brightening ingredients deeper into the skin to reduce pigmentation.
- Lasers – Low-energy lasers, such as PicoSure or Q-switched lasers, can break down pigment without damaging surrounding skin. However, laser treatments must be done cautiously to avoid stimulating melanocytes.
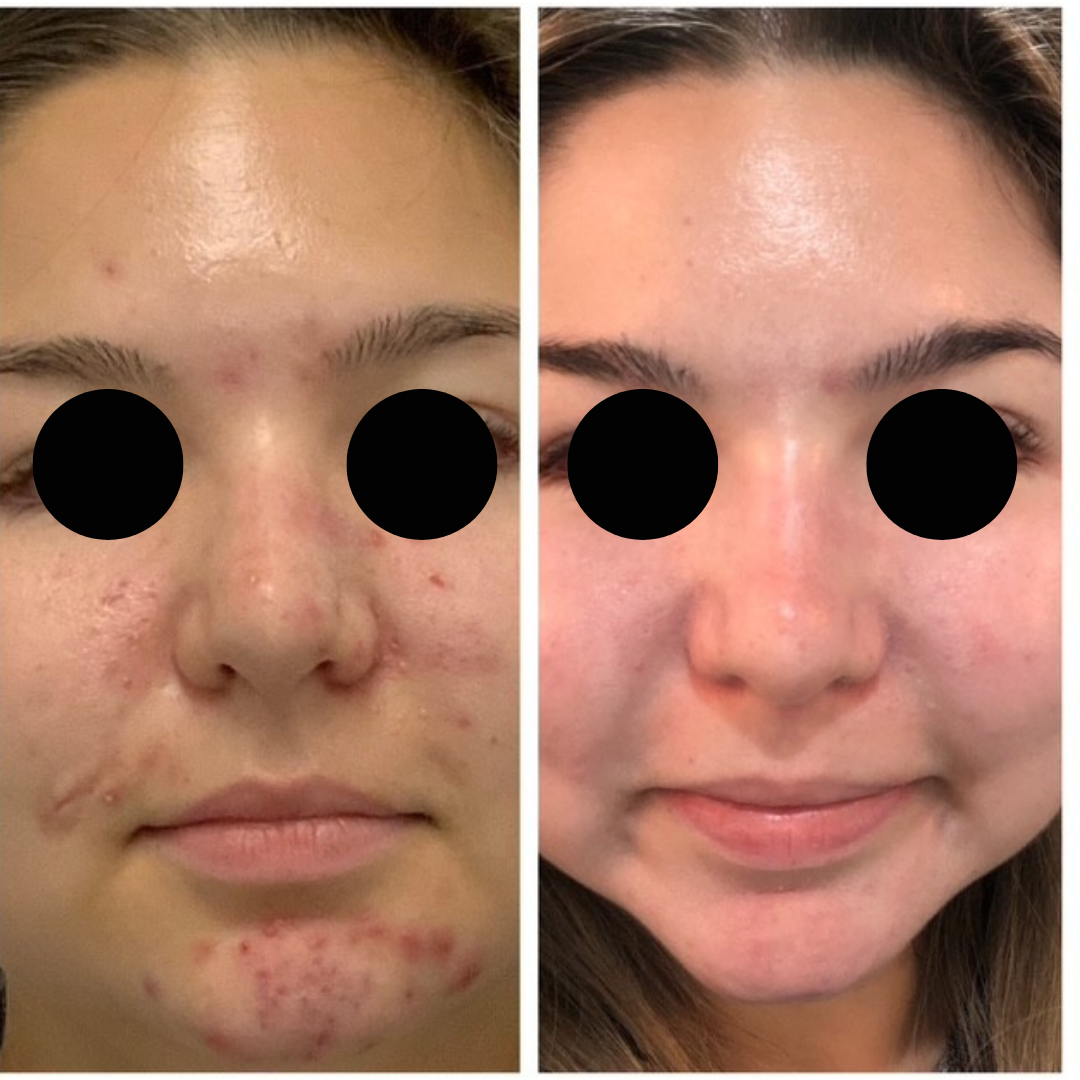
Expert Insight from JoAnn Francis
JoAnn Francis has worked with countless clients over the years, successfully treating melasma and helping them maintain clear, even-toned skin with a carefully designed professional skincare regimen. Her customized protocols address the root causes of melasma and include high-quality, pharmaceutical-grade products to manage pigmentation effectively.
If you’re struggling with melasma and want to see real results, JoAnn Francis can create a personalized skincare plan tailored to your skin’s unique needs. Reach out for a free online consultation to discover how you can regain smooth, even skin and keep melasma under control.
Final Thoughts
While melasma can be stubborn and challenging, consistent use of sunscreen, tyrosinase inhibitors, and prescription treatments can significantly improve skin tone and texture. Controlling inflammation, protecting your skin from UV and heat, and maintaining a strong skin barrier are key to long-term management. A personalized skincare routine and guidance from a professional like JoAnn Francis can help you keep melasma under control and maintain radiant, even-toned skin.





Comments